Perioperative Combination Therapy Identifies Responders in Early HER2+ Breast Cancer
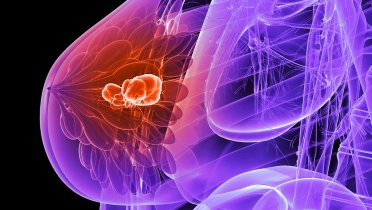
A new study published in Clinical Cancer Research has found that combined therapy with lapatinib and trastuzumab between diagnosis and surgery inhibits disease proliferation in patients with early HER2-positive breast cancer.
Equally important, an early response after such short-duration, anti-HER2 dual therapy aids in the identification of cancers that are dependent on the HER2 pathway, a finding the researchers said may ultimately provide a strategy for exploring risk-adapted individualized treatment options in these patients.
Trastuzumab inhibits function of the HER2 protein, while lapatinib has been shown to block the HER1/2 internal tyrosine kinase domain and inhibit proliferation of HER2-positive cancers.
Changes in proliferation biomarkers such as Ki67 have been found to predict clinical response and long-term outcome following short-term endocrine therapy in estrogen receptor-positive breast cancer.
In the phase 2 EPHOS-B study, researchers sought to determine whether perioperative anti-HER2 therapy inhibits proliferation and/or increases apoptosis in HER2-positive breast cancer—and included 257 women with newly diagnosed HER2-positive invasive breast cancer, all of whom were scheduled to undergo surgery.
In the first part of the 2-part study, participants were randomized to either no treatment (controls; n = 22), trastuzumab (n = 57), or lapatinib (n = 51). In part 2, 29 patients served as controls, 32 received trastuzumab alone, and 66 were treated with combination trastuzumab-lapatinib. In all cases, patients were treated for 11 days prior to surgery.
According to lead author Nigel Bundred, MD, from the department of academic surgery the Manchester University Foundation Trust, UK, Ki67 response was evaluable in a total of 223 patients. In part 1, Ki67 response occurred in 66% (29/44) lapatinib patients, compared with 37% (18/49) of those receiving trastuzumab (P = .007) and 5% of controls (1/22; P < .0001).
In part 2, Ki67 response was observed in 74% of patients (36/49) who received combination trastuzumab-lapatinib therapy versus 45% of those (14/31) treated with trastuzumab alone (P = .02) and 7% of controls (2/28; P < .0001). On the other hand, no significant increase in apoptosis was seen in any treatment group after 11 days of therapy.
Six patients achieved complete pathologic response (residual cancer burden = 0), while 13 achieved minimal residual disease (residual cancer burden = 1). Seventeen of these 19 cases were among patients who received combination therapy.
Over a 6-year median follow-up period, 28 patients (11%) had disease recurrence, while 19 (7%) died. Interestingly, however, no recurrences or deaths were observed among patients who achieved a pathologic complete response. Similarly, decreases in Ki67 percentage of at least 50% were associated with fewer cases of disease recurrence (P = .002).
Given these results, the researchers concluded that early response following short-duration anti-HER2 dual therapy can identify cases of breast cancer that are dependent on the HER2 pathway, a finding that may open the door to individualized treatment for these patients.
“The data we report on the early disappearance of tumors 11 days after treatment commencement may identify a patient group highly sensitive to the HER2-pathway who can potentially avoid chemotherapy altogether,” Bundred and colleagues concluded.
Reference:
https://aacrjournals.org/clincancerres/article/28/7/1323/682200/Combined-Perioperative-Lapatinib-and-Trastuzumab
Disclosures: Authors declared financial ties to drugmakers; see full study for details.
Photo Credit: Getty Images, Pixabay
By Michael Vlessides, MD /alert Contributor
.jpg)











.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)

.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
_.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)


.jpg)
.jpg)
.jpg)
.jpg)




.jpg)


.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)



.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)


.jpg)

.jpg)
.jpg)

.jpg)

.jpg)


.jpg)
.jpg)
.jpg)
 Featured Breast Cancer Videos
Featured Breast Cancer Videos.jpg)