Loading the player...
Durvalumab Provokes Robust Long-Term Outcomes in Patients with TNBC
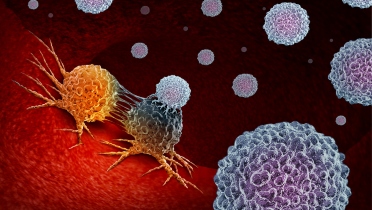
The addition of the immune checkpoint inhibitor durvalumab to standard neoadjuvant chemotherapy resulted in significant long-term survival improvements in patients with triple-negative breast cancer, according to study results presented at the ASCO Annual Meeting.
The benefit seen with durvalumab was robust, even though pathologic complete response (pCR) increases were modest and treatment did not continue following surgery, according to the researchers.
A previously published report from the phase 2 GeparNuevo trial showed that durvalumab, an anti–PD-L1 immunotherapy, exhibited particular activity in patients treated with durvalumab monotherapy prior to standard neoadjuvant chemotherapy (window phase).
In the study, the researchers randomly assigned patients with TNBC to a 2-week course of intravenous durvalumab (0.75 g) or placebo, followed by durvalumab or placebo plus standard chemotherapy.
The primary endpoint of the study was pCR rate. Secondary time-to-event endpoints included invasive disease-free survival (iDFS), distant disease-free survival (dDFS) and overall survival (OS).
In the overall cohort (n = 174), the pCR rate favored durvalumab over placebo (53.4% vs. 44.2%; odds ratio [OR], 1.45; 95% CI, 0.8-2.63). The effect of durvalumab on pCR was significant only among patients who participated in the window phase (61% vs. 41.4%; OR, 2.22; 95% CI, 1.06-4.64; P = .035; interaction P = .048).
The median follow up was 42.2 months, during which 34 events were recorded. Compared with patients who did not respond, patients in pCR achieved a significantly higher 3-year iDFS rate (92% vs. 71.9%; log-rank P = .002). The 3-year iDFS rate also improved among patients assigned durvalumab (84.9% vs. 76.9%; hazard ratio, 0.54; 95% CI, 0.27-1.09).
Treatment with durvalumab provoked significantly higher rates of 3-year dDFS (91.4% vs. 79.5%; P = .0148) and OS (95.1% vs. 83.1%; P = .0076). The researchers reported no difference in 3-year iDFS, dDFS or OS based on participation in the window phase.
Patients were stratified by stromal tumor-infiltrating lymphocytes. The researchers previously reported a significant association between high stromal tumor-infiltrating lymphocytes and increased pCR.
Given the vigorous long-term outcomes observed with neoadjuvant durvalumab, “it needs to be questioned whether adjuvant therapy with [immune checkpoint inhibitors] is needed at all,” the researchers concluded.
By Cameron Kelsall, /alert Contributor
The benefit seen with durvalumab was robust, even though pathologic complete response (pCR) increases were modest and treatment did not continue following surgery, according to the researchers.
A previously published report from the phase 2 GeparNuevo trial showed that durvalumab, an anti–PD-L1 immunotherapy, exhibited particular activity in patients treated with durvalumab monotherapy prior to standard neoadjuvant chemotherapy (window phase).
In the study, the researchers randomly assigned patients with TNBC to a 2-week course of intravenous durvalumab (0.75 g) or placebo, followed by durvalumab or placebo plus standard chemotherapy.
The primary endpoint of the study was pCR rate. Secondary time-to-event endpoints included invasive disease-free survival (iDFS), distant disease-free survival (dDFS) and overall survival (OS).
In the overall cohort (n = 174), the pCR rate favored durvalumab over placebo (53.4% vs. 44.2%; odds ratio [OR], 1.45; 95% CI, 0.8-2.63). The effect of durvalumab on pCR was significant only among patients who participated in the window phase (61% vs. 41.4%; OR, 2.22; 95% CI, 1.06-4.64; P = .035; interaction P = .048).
The median follow up was 42.2 months, during which 34 events were recorded. Compared with patients who did not respond, patients in pCR achieved a significantly higher 3-year iDFS rate (92% vs. 71.9%; log-rank P = .002). The 3-year iDFS rate also improved among patients assigned durvalumab (84.9% vs. 76.9%; hazard ratio, 0.54; 95% CI, 0.27-1.09).
Treatment with durvalumab provoked significantly higher rates of 3-year dDFS (91.4% vs. 79.5%; P = .0148) and OS (95.1% vs. 83.1%; P = .0076). The researchers reported no difference in 3-year iDFS, dDFS or OS based on participation in the window phase.
Patients were stratified by stromal tumor-infiltrating lymphocytes. The researchers previously reported a significant association between high stromal tumor-infiltrating lymphocytes and increased pCR.
Given the vigorous long-term outcomes observed with neoadjuvant durvalumab, “it needs to be questioned whether adjuvant therapy with [immune checkpoint inhibitors] is needed at all,” the researchers concluded.
By Cameron Kelsall, /alert Contributor











.jpg)
.jpg)

.jpg)
.jpg)

.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)




.jpg)
.jpg)

.jpg)
.jpg)
.jpg)

.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)

.jpg)
.jpg)


.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
_.jpg)



.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)

.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)


.jpg)

.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
 Featured Breast Cancer Videos
Featured Breast Cancer Videos.jpg)