Loading the player...
Nobel Prize Winner Links Cancer Immunotherapy to Programmed Cell Death Gene
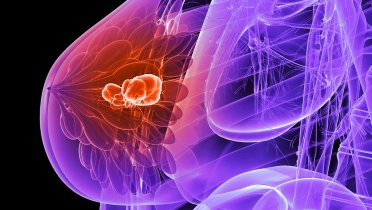
The BIRC2 gene, responsible for turning off a cell’s programmed death signals may also be responsible in making breast cancer and melanoma cells resistant to immunotherapies that fight cancer, according to new research from Gregg Semenza, MD, PhD, and fellow Johns Hopkins Medicine researchers.
When the gene goes into overdrive, it causes an overexpression of protein levels that occurs in around 40% of breast cancers—particularly triple negative BC, according to a press release from Johns Hopkins. BIRC2 overexpression could be a key marker for immunotherapy resistance, according to the researchers.
Semenza shared the 2019 Nobel Prize in Physiology or Medicine, for the discovery of the gene that guides cell adaption to low oxygen levels, a condition called hypoxia. His team defined how hypoxia shapes cancer cell survival.
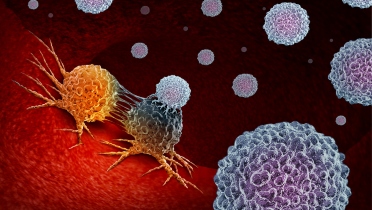
A cell surface protein, CD47, signals the blocking of cancer cell death using immune cells called macrophages. Semenza believes these “super-survivor cancer cells” could explain why many cancer patients respond to drugs that boost the immune system’s ability to target cancer cells, according to the release.
In the current study published in Cell Reports—his team utilized 325 human genes identified at the Dana Farber Cancer Institute—with overexpressed protein products in melanoma cells and “linked to processes that help cancer cells evade the immune system.”
They identified 38 genes, including BIRC2, that are influenced by the transcription factor HIR-1, which regulates how cells adapt to hypoxia. They found that hypoxia proteins HIF1 and HIF2 bind directly to the BIRC2 gene in low oxygen conditions.
The team injected mice with human breast cancer or melanoma cells genetically engineered to contain little or no BIRC2 gene expression. In mice with cancer cells lacking BIRC2 expression, tumors were slower to form, at about three to four weeks vs. the average two weeks to form tumors in mice.
Additionally, the tumors formed by BIRC2-free cancer cells had up to five times the level of the protein CXCL9, which attracts immune system T-cells. They found the longer the tumor took to form, the more T-cells were present inside the tumor.
Semenza’s team injected the BIRC2-free melanoma and BC cells into mice bred to have no functioning immune system. In these mice, tumors grew at the same rate in about two weeks, as typical tumors.
"This suggests that the decreased tumor growth rate associated with loss of BIRC2 is dependent on recruiting T-cells and natural killer cells into the tumor," Gregg Semenza, MD, PhD, the C. Michael Armstrong Professor of Genetic Medicine, Pediatrics, Oncology, Medicine, Radiation Oncology and Biological Chemistry at the Johns Hopkins University School of Medicine, and director of the Vascular Program at the Johns Hopkins Institute for Cell Engineering, said in the release.
Next, his team analyzed mice implanted with human BC or melanoma tumors that produced BIRC2 or was engineered to lack the gene. They administered the mice with immunotherapy drugs appropriate for each cancer. The immunotherapy drugs were effective only against the tumors that lacked BIRC2.
By MD /alert Staff
When the gene goes into overdrive, it causes an overexpression of protein levels that occurs in around 40% of breast cancers—particularly triple negative BC, according to a press release from Johns Hopkins. BIRC2 overexpression could be a key marker for immunotherapy resistance, according to the researchers.
Semenza shared the 2019 Nobel Prize in Physiology or Medicine, for the discovery of the gene that guides cell adaption to low oxygen levels, a condition called hypoxia. His team defined how hypoxia shapes cancer cell survival.
A cell surface protein, CD47, signals the blocking of cancer cell death using immune cells called macrophages. Semenza believes these “super-survivor cancer cells” could explain why many cancer patients respond to drugs that boost the immune system’s ability to target cancer cells, according to the release.
In the current study published in Cell Reports—his team utilized 325 human genes identified at the Dana Farber Cancer Institute—with overexpressed protein products in melanoma cells and “linked to processes that help cancer cells evade the immune system.”
They identified 38 genes, including BIRC2, that are influenced by the transcription factor HIR-1, which regulates how cells adapt to hypoxia. They found that hypoxia proteins HIF1 and HIF2 bind directly to the BIRC2 gene in low oxygen conditions.
The team injected mice with human breast cancer or melanoma cells genetically engineered to contain little or no BIRC2 gene expression. In mice with cancer cells lacking BIRC2 expression, tumors were slower to form, at about three to four weeks vs. the average two weeks to form tumors in mice.
Additionally, the tumors formed by BIRC2-free cancer cells had up to five times the level of the protein CXCL9, which attracts immune system T-cells. They found the longer the tumor took to form, the more T-cells were present inside the tumor.
Semenza’s team injected the BIRC2-free melanoma and BC cells into mice bred to have no functioning immune system. In these mice, tumors grew at the same rate in about two weeks, as typical tumors.
"This suggests that the decreased tumor growth rate associated with loss of BIRC2 is dependent on recruiting T-cells and natural killer cells into the tumor," Gregg Semenza, MD, PhD, the C. Michael Armstrong Professor of Genetic Medicine, Pediatrics, Oncology, Medicine, Radiation Oncology and Biological Chemistry at the Johns Hopkins University School of Medicine, and director of the Vascular Program at the Johns Hopkins Institute for Cell Engineering, said in the release.
Next, his team analyzed mice implanted with human BC or melanoma tumors that produced BIRC2 or was engineered to lack the gene. They administered the mice with immunotherapy drugs appropriate for each cancer. The immunotherapy drugs were effective only against the tumors that lacked BIRC2.
By MD /alert Staff
.jpg)











.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)


.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)

.jpg)
.jpg)
.jpg)
.jpg)


.jpg)
.jpg)

.jpg)

.jpg)

.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)


.jpg)
.jpg)


.jpg)
.jpg)

.jpg)


.jpg)
.jpg)
.jpg)

.jpg)
.jpg)

.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)

_.jpg)
.jpg)
.jpg)
.jpg)
 Featured Breast Cancer Videos
Featured Breast Cancer Videos.jpg)